✔ 100% Authentic Product
👁️ Currently Viewing 2812
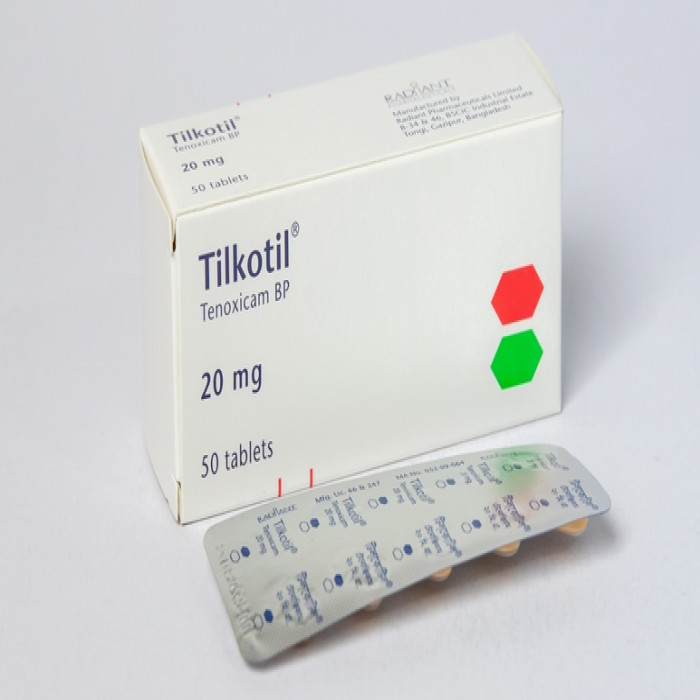
Tenoxicam is used for the treatment of Osteoarthritis, Rheumatoid Arthritis, Spine Arthritis, Gout, Soft Tissues Disorders, and other conditions.
Discount
Price: ৳ 77
MRP:
৳
80.86
5%
Off

100% Genuine Products, Guaranteed

Safe & Secure Payments, Always
Fast, Secure & Efficient Delivery
Proper Packaging
 Cash on Delivery - All over Bangladesh
Cash on Delivery - All over Bangladesh Regular Delivery - 12-24 Hours, Dhaka City* Charge Tk.39-59
Regular Delivery - 12-24 Hours, Dhaka City* Charge Tk.39-59 Regular Delivery - 24-48 Hours, Other Cities* Charge Tk.99-110
Regular Delivery - 24-48 Hours, Other Cities* Charge Tk.99-110
🌙 রমযান অফার 🌙
 ফ্রি ডেলিভারিঃ - ৭৯৯ টাকা+ অর্ডারে, ঢাকা
শহরে
ফ্রি ডেলিভারিঃ - ৭৯৯ টাকা+ অর্ডারে, ঢাকা
শহরে ফ্রি ডেলিভারিঃ - ২৭৯৯ টাকা+ অর্ডারে, ঢাকার
বাহিরে
ফ্রি ডেলিভারিঃ - ২৭৯৯ টাকা+ অর্ডারে, ঢাকার
বাহিরে
📲 মোবাইল অ্যাপ অর্ডারে সাশ্রয় বেশী
-
Google Play Store থেকে ডাউনলোড
-
Apple Store থেকে ডাউনলোড
100% Genuine Products, Guaranteed
Safe & Secure Payments, Always
Fast, Secure & Efficient Delivery
Proper Packaging
 Cash on Delivery - All over Bangladesh
Cash on Delivery - All over Bangladesh Regular Delivery - 12-24 Hours, Dhaka City* Charge Tk.39-59
Regular Delivery - 12-24 Hours, Dhaka City* Charge Tk.39-59 Regular Delivery - 24-48 Hours, Other Cities* Charge Tk.99-110
Regular Delivery - 24-48 Hours, Other Cities* Charge Tk.99-110 ফ্রি ডেলিভারিঃ - ৭৯৯ টাকা+ অর্ডারে, ঢাকা
শহরে
ফ্রি ডেলিভারিঃ - ৭৯৯ টাকা+ অর্ডারে, ঢাকা
শহরে ফ্রি ডেলিভারিঃ - ২৭৯৯ টাকা+ অর্ডারে, ঢাকার
বাহিরে
ফ্রি ডেলিভারিঃ - ২৭৯৯ টাকা+ অর্ডারে, ঢাকার
বাহিরে- Google Play Store থেকে ডাউনলোড
- Apple Store থেকে ডাউনলোড
🌙 রমযান অফার 🌙
📲 মোবাইল অ্যাপ অর্ডারে সাশ্রয় বেশী
✅ Description:
Tenorix 20mg Tablet is an analgesic which is used to relieve
- Rheumatoid Arthritis
- Osteoarthritis
- Ankylosing Spondylitis
- Acute Gout
- Post-operative pain
- Primary Dysmenorrhea
Safety Advices
Alcohol
UNSAFE
Concurrent use of alcohol with Tenorix 20mg Tablet may lead to increased sedation, drowsiness, dizziness, impaired coordination, and other side effects. It is advisable to avoid alcohol while taking Tenorix 20mg Tablet. Patients should consult their healthcare provider for personalized advice.
Pregnancy
UNSAFE
Limited human studies are available, but animal studies suggest potential harm to the developing baby. Pregnant individuals should consult their doctor before using Tenorix 20mg Tablet. The doctor will assess the benefits versus potential risks before prescribing.

Breastfeeding
CONSULT YOUR DOCTOR
Breastfeeding individuals should consult their doctor to evaluate the potential risks and benefits before using Tenorix 20mg Tablet.
Driving
CAUTION
Caution is advised while driving. Individuals experiencing these side effects should refrain from driving. Side effects such as tiredness, drowsiness, dizziness, visual disturbances, and balance issues can affect the ability to drive safely.

Kidey
CONSULT YOUR DOCTOR
Dose adjustment may be necessary in individuals with kidney impairment. Consultation with a doctor is essential, and Tenorix 20mg Tablet may not be recommended in cases of severe kidney disease.
Liver
CONSULT YOUR DOCTOR
Dose adjustment may be necessary in individuals with liver impairment. Consultation with a doctor is essential, and Tenorix 20mg Tablet may not be recommended in cases of severe liver disease.
✔️ Osteoarthritis
Osteoarthritis is a prevalent form of arthritis that affects millions of people globally. It occurs when the protective cartilage covering the ends of bones gradually deteriorates, primarily affecting joints such as hands, knees, spine, and hips. This chronic condition involves the biochemical breakdown of cartilage in synovial joints, leading to symptoms like joint pain, soreness, and inflammation, usually progressing slowly.
There are two main types of osteoarthritis: primary and secondary. Primary osteoarthritis is commonly associated with aging and wear and tear on joints over time, typically emerging around the age of 55 or 60. Secondary osteoarthritis is triggered by conditions that alter the joint environment, such as severe trauma, genetic anomalies, metabolic issues, allergies, and diseases like rheumatoid arthritis or gout.
Causes of osteoarthritis include age-related wear and tear on cartilage, joint injuries, and continuous stress on joints due to occupation or sports. The symptoms of osteoarthritis, such as joint pain, stiffness, decreased flexibility, bone growth, and swelling, tend to worsen gradually over time.
Risk factors for osteoarthritis include increasing age, gender (more common in women), weight gain, joint damage, continuous joint pressure, genetics, bone anomalies, and specific metabolic conditions.
Preventive measures involve weight management, regular exercise, avoiding injuries, and adopting a healthy lifestyle. Treatment options aim to manage symptoms and improve joint function. Medications, physical therapy, and, in severe cases, surgical interventions like joint replacement may be considered.
Diagnosis involves a physical examination, imaging tests (X-rays, MRI), and sometimes lab tests to rule out other conditions. Complications of osteoarthritis include cartilage degradation, bone death, stress fractures, and internal joint bleeding.
Home remedies for osteoarthritis include learning about the condition, exercising, movement therapies like tai chi and yoga, and using heat or cold packs. A balanced diet with foods like brown rice, green vegetables, fruits, and specific herbs may help manage symptoms. Certain foods like animal protein, dairy, eggs, and processed foods should be avoided.
Medications for osteoarthritis include acetaminophen, NSAIDs, and duloxetine for pain management. Recovery from osteoarthritis involves post-treatment guidelines like avoiding heavy exercise, using heat or cold packs, seeking assistance, getting adequate rest, and maintaining a positive outlook.
✔️ Rheumatoid Arthritis
Rheumatoid Arthritis is an autoimmune disorder characterized by the immune system attacking the body's healthy tissues, particularly the joint linings. This results in inflammation of the joints, leading to pain and swelling. If left untreated, it can adversely affect the joint structure, causing deformities and bone erosion. In contrast to osteoarthritis, which primarily affects the joints, rheumatoid arthritis can also damage other organs and tissues.
The condition progresses through four stages:
- Stage 1: Early inflammation of the synovium, causing joint pain without damage to the joint itself.
- Stage 2: Moderate stage involving cartilage damage, leading to joint stiffness and reduced mobility.
- Stage 3: Inflammation wears out cartilage and bone ends, resulting in joint instability, deformities, and increased pain.
- Stage 4: Severe stage where joints are extensively damaged, leading to pain, swelling, stiffness, muscle weakness, and limited motion. Joint replacement may be considered at this stage.
Rheumatoid arthritis can affect various non-joint structures and organs, including the skin, eyes, lungs, heart, kidneys, salivary glands, nerve tissue, bone marrow, and blood vessels. Early signs of the condition include fatigue, low-grade fever, weight loss, morning stiffness, joint tenderness, pain, swelling, redness, warmth, numbness, tingling, and decreased mobility.
Several factors contribute to rheumatoid arthritis, such as exposure to bacteria with periodontal disease, bone injuries, genetic predisposition (though not a dominant factor), hormonal imbalances (more common in women due to estrogen imbalance), and smoking.
Diagnosis involves a physical examination checking for joint abnormalities, strength, and reflexes. Blood tests, such as erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP), may indicate inflammation. Imaging techniques like X-rays, ultrasound, and MRI help assess joint damage. Occupational or physiotherapy may be recommended to maintain joint flexibility.
While there is no cure for rheumatoid arthritis, treatment aims to manage symptoms and slow disease progression. This may involve dietary changes, exercise routines, medications, and home remedies. The treat-to-target approach is commonly used to control inflammation and prevent joint and organ damage.
Rheumatoid arthritis doesn't typically go into full remission, but symptoms can be managed with medications and lifestyle adjustments. Abruptly discontinuing medication is not advisable, and any changes should be discussed with a healthcare professional due to the progressive nature of the disease.
✔️ Ankylosing Spondylitis
Ankylosing Spondylitis is a type of arthritis that predominantly affects the spine, causing stiffness and pain from the lower back to the neck. The condition is characterized by the fusion of vertebrae, resulting in rigid bones. Early diagnosis and treatment are crucial for managing symptoms, controlling stiffness and pain, and preventing significant deformities. Ankylosing spondylitis may manifest with symptoms such as back and neck pain, fatigue, stiffness in the lower back, blurred vision, inflammation of the eyes, inflamed tendons, sleep disorders, and physical deformities.
Distinguishing between spondylitis and ankylosing spondylitis reveals differences in the damage caused to bones and joints. Spondylitis typically involves inflammation between spinal joints, leading to fusing and difficulties in movement. Conversely, spondylosis entails wear and tear on joints, progressing with age and potentially causing stiffness and pain due to disk degeneration or bone spurs.
The causes of ankylosing spondylitis remain unknown, but there is a strong hereditary link, with the HLA-B27 gene being implicated. However, around 10% of individuals with this gene show no symptoms. Diagnosis involves various methods, including X-rays, chest measurements during breathing, and lab tests, as general diagnostic testing may not be conclusive.
While there is no cure for ankylosing spondylitis, symptomatic treatments aim to alleviate pain, and stiffness, and prevent deformities. Physical and occupational therapy play essential roles in maintaining body function and minimizing severe deformities. Therapists may recommend customized exercise regimes, with swimming and breathing techniques being highly advised.
The best treatment for ankylosing spondylitis involves a multi-faceted approach:
Medications: Anti-inflammatory drugs, such as NSAIDs, or more advanced medications like TNF blockers and IL-17 inhibitors, help manage pain, stiffness, and inflammation.
Therapy: Physical and occupational therapy, including specific exercises and postural recommendations, contributes to pain relief and improved flexibility.
Surgery: While not the first choice, surgery may be recommended in cases of severe joint damage requiring replacement.
Home Care: Home remedies like heat or cold compresses, baths, and supportive pads can provide relief.
While ankylosing spondylitis cannot be permanently cured, medical treatments can help manage symptoms and slow bone fusion. The condition is considered serious, potentially leading to complications such as eye inflammation, impaired vision, fatigue, osteoporosis, gastrointestinal disorders, increased cardiovascular risk, cauda equina syndrome, and amyloidosis.
Ankylosing spondylitis may qualify as a disability due to its impact on mobility and daily activities, causing discomfort and pain. Symptoms like persistent and severe back pain, blurred vision, or extreme nighttime or morning pain warrant immediate medical attention.
Dietary adjustments can contribute to recovery, with a focus on colorful, antioxidant-rich foods, whole grains, omega-3 fatty acids, and calcium and vitamin D sources. Conversely, individuals with ankylosing spondylitis should limit their intake of sugar, red meat, salt, high-fat foods, alcohol, wheat and gluten, and certain dairy products.
Exercise plays a crucial role in managing spondylitis, and recommended exercises include press-ups, wall sits, planks, standing leg raises, chin tucks, shoulder rolls, hip stretches, and corner stretches. These exercises are designed to improve flexibility, strengthen muscles, and alleviate pain.
In summary, ankylosing spondylitis is a complex condition that requires a comprehensive approach to treatment, involving medications, therapy, surgery when necessary, and lifestyle modifications. Early diagnosis and management are key to improving outcomes and maintaining a better quality of life for individuals with ankylosing spondylitis.
✔️ Gout
Gout is the most common type of inflammatory arthritis, characterized by sudden and intense joint pain, often affecting the big toe. It can also impact other joints such as those in the ankle, knee, or fingers. Men are more prone to gout, with the risk increasing after the age of 40, while women are more susceptible after menopause. Gout results from the accumulation of uric acid crystals in the joints, causing pain and swelling.
Causes of Gout: Gout develops in individuals with high levels of uric acid, which can be due to the breakdown of purines found in cells and certain foods. Foods rich in purines include red meat, organic meats, seafood, sugary sodas, and beer. When uric acid accumulates, it forms needle-like crystals that lodge in joints, leading to sudden and severe pain and swelling.
Risk Factors for Gout: Several factors increase the likelihood of developing gout:
- High consumption of purine-rich foods
- Intake of high-fructose corn syrup and excessive alcohol, especially beer
- Being overweight
- Family history of gout
- Chronic conditions like diabetes, obesity, heart, or kidney disease
- Use of certain medications, including diuretics and beta blockers
- Imbalance in the microbiome, which regulates the immune system
Diagnosing Gout: Diagnosis involves a combination of medical history, a physical exam, and tests. Key diagnostic procedures include:
- Joint fluid analysis: Withdrawal of fluid from the affected joint to examine uric acid crystals under a microscope.
- Blood test: Checking uric acid levels, though normal levels do not rule out gout.
- Imaging tests: X-rays, ultrasound, MRI, and dual-energy CT to visualize uric acid crystals in joints.
Treatments for Gout: The treatment plan for gout depends on the frequency and severity of symptoms:
- Lifestyle changes: Weight loss and adopting a healthy diet, such as the Mediterranean or DASH diet, can help prevent gout attacks.
- Anti-inflammatories: NSAIDs like ibuprofen and naproxen, colchicine, and corticosteroids are prescribed to alleviate pain and inflammation during attacks.
- Uric acid-lowering drugs: For recurrent gout attacks, tophi, or joint damage, medications like allopurinol are recommended. A treat-to-target approach, aiming for a specific uric acid level, is often adopted.
✔️ Side Effects of Tenorix 20mg:
Common side effects include gastrointestinal discomfort, dyspepsia, headache, dizziness, and nausea. Less common side effects may include constipation, diarrhea, stomatitis, gastritis, vomiting, ulcers, and elevated liver enzymes.
✔️ Pharmacology:
Tenorix 20 mg is a non-steroidal anti-inflammatory drug (NSAID) with anti-inflammatory, analgesic, and antipyretic properties. It also inhibits platelet aggregation and prostaglandin biosynthesis, making it effective in treating inflammatory and degenerative disorders of the musculoskeletal system.
✔️ Dosage & Administration of Tenorix 20 mg:
- For most indications (except primary dysmenorrhea, post-operative pain, and acute gout), the usual recommended dose is 20 mg once daily.
- In rheumatoid arthritis, it should be taken at night to relieve morning stiffness.
- The recommended dose for primary dysmenorrhea is 20 to 40 mg once daily.
- For post-operative pain, the recommended dose is 40 mg once daily for up to five days.
- In acute gout, the recommended dose is 40 mg once daily for two days followed by 20 mg once daily for a further five days.
✔️ Administration:
The tablets should be taken with a glass of water and preferably during or immediately after a meal.
✔️ Pediatric Uses:
Not recommended for use in patients under 16 years of age.
✔️ Overdose Effects:
While acute overdosage is rare, signs and symptoms may include those mentioned as undesirable effects. Conventional measures to reduce the absorption and speed up elimination should be employed.
✔️ Mode Of Action:
Tenorix 20 mg is an NSAID that inhibits prostaglandin biosynthesis, providing anti-inflammatory, analgesic, and antipyretic effects. It also inhibits platelet aggregation and metalloproteinases associated with cartilage breakdown.
✔️ Interaction of Tenorix 20mg:
- Interaction with salicylate may increase the risk of gastrointestinal reactions.
- Caution is advised when co-administering with methotrexate, as it may reduce its renal tubular secretion.
- Potential interactions with lithium, K-sparing diuretics, antihypertensive drugs, and others should be monitored closely.
✔️ Contraindications:
Tenorix 20 mg is contraindicated in patients:
- Hypersensitive to the drug
- With asthma, rhinitis, or urticaria induced by salicylates or other NSAIDs
- With upper gastrointestinal tract diseases such as gastritis, gastric, and duodenal ulcers
✔️ Pregnancy & Lactation:
The safety of Tenorix 20 mg during pregnancy is not well-established, and caution is advised. It should not be used during lactation due to insufficient information about its safety.
✔️ Precautions & Warnings:
- Monitoring of renal and cardiac function is necessary, especially in patients with pre-existing conditions.
- Tenorix 20 mg may inhibit platelet aggregation, requiring caution in patients with coagulation disorders.
- Careful observation is recommended if symptoms of gastrointestinal disease develop.
- Visual disturbances may occur, necessitating ophthalmic evaluation.
✔️ Storage Conditions:
Store below 30°C, protect from light and moisture and keep out of reach of children.
⚠️Disclaimer:
At ePharma, we’re committed to providing accurate and accessible health information. However, all content is intended for informational purposes only and should not replace medical advice from a qualified physician. Please consult your healthcare provider for personalized guidance. We aim to support, not substitute, the doctor-patient relationship.